One in eight people on earth now lives with obesity. Rates have doubled in adults, quadrupled in adolescents, and are on track to become one of the most expensive public health crises of the century. Yet beneath the rising numbers, something deeper is shifting. The world is rethinking what obesity is and what fighting it truly requires.
Across continents, the response has grown more urgent and more layered. Pharmaceutical companies are producing emotionally charged campaigns that dismantle stigma. Governments are rewriting food policy through taxes and warning labels. International health bodies are creating new diagnostic frameworks that move past BMI and reclassify obesity as Adiposity-Based Chronic Disease, or ABCD.
Obesity is being redefined, medically and culturally.
And the most revealing window into this reset is the variety of campaigns emerging today.
From Eli Lilly’s hard-hitting films on shame and misuse of medication to Novo Nordisk’s multi-country destigmatization strategy to national programs in Mexico and the UK and WHO’s policy-driven acceleration plans, each campaign reflects a different philosophy of how obesity should be understood, prevented, and treated.
These campaigns shape more than awareness.
They influence policy, medical language, cultural narratives, and the pathways to care. Understanding them helps us understand how the global fight will evolve in the decade ahead.
The Pharmaceutical Industry's Response to Obesity
Eli Lilly's "Get Better" Campaign
Eli Lilly has placed itself at the front of obesity education with its “Get Better” platform. Built to reinforce the idea that obesity is a serious disease, not a personal failing, the campaign uses two emotionally charged films titled “Shame” and “Big Night.”
“Shame,” launched during Obesity Care Week, follows a woman moving through a muted, black and white world filled with judgement from strangers and family. The voiceover directly challenges stigma around weight and the use of GLP 1 medications. The message is clear: obesity is a disease. Shame has no place in its treatment.

GLP-1 medications are a class of therapies that regulate appetite, blood sugar, and insulin response, making them one of the most effective modern treatments for obesity.
“Big Night,” released during awards season, tackles the growing misuse of anti obesity medication for cosmetic weight loss. The 30-second film bluntly calls out people using the drugs to fit into a dress or tux. The goal is to protect access for those who need medication like Zepbound and Mounjaro for genuine metabolic treatment.
Beyond film, Lilly partnered with the Obesity Action Coalition to develop a library of respectful, realistic images of people with obesity, countering decades of dehumanizing media portrayals.
Lilly is also advancing pharmaceutical options. It is developing orforglipron, an investigational oral GLP 1 therapy designed for early intervention and long term management, offering a more convenient alternative to injectables.

Novo Nordisk's Multi-Layered Approach
Novo Nordisk, Lilly’s most direct competitor, has rolled out a series of global campaigns built on empathy and stigma reduction.
Its flagship initiative, “It’s Bigger Than Me,” aims to shift cultural narratives around weight through human-centric storytelling. The campaign’s tone is intentionally balanced. It respects body positivity while emphasizing obesity as a health condition that deserves medical attention. The reach was significant. More than 26 million viewers. More than 7 million engagements. High video completion rates. Heavy website traffic.
Novo has also launched demographic-specific campaigns.
“Share the Weight” focuses on young people and highlights that two-thirds of teenagers living with obesity believe they must manage it alone.
“Believe On,” for Wegovy, speaks directly to healthcare professionals and celebrates patient resilience.

But even thoughtful campaigns can misfire.
A Spanish awareness campaign, built around the line “obesity can kill,” was widely criticized for fear based messaging that risked reinforcing stigma rather than reducing it.
Beyond marketing, Novo Nordisk’s partnership with UNICEF has focused on creating healthier environments for children in Latin America, the Caribbean, and East Asia, tackling obesity at its roots.
Government-Led Initiatives to Fight Obesity
Mexico's Sugar Tax and “First Obesity, Then Diabetes”
Facing one of the world’s highest obesity rates, Mexico implemented a bold health strategy in 2014. The country introduced a national sugar tax and launched the highly visual “Primero Obesidad, Luego Diabetes” campaign. The ads showed long term health consequences of excess sugar consumption in stark detail.
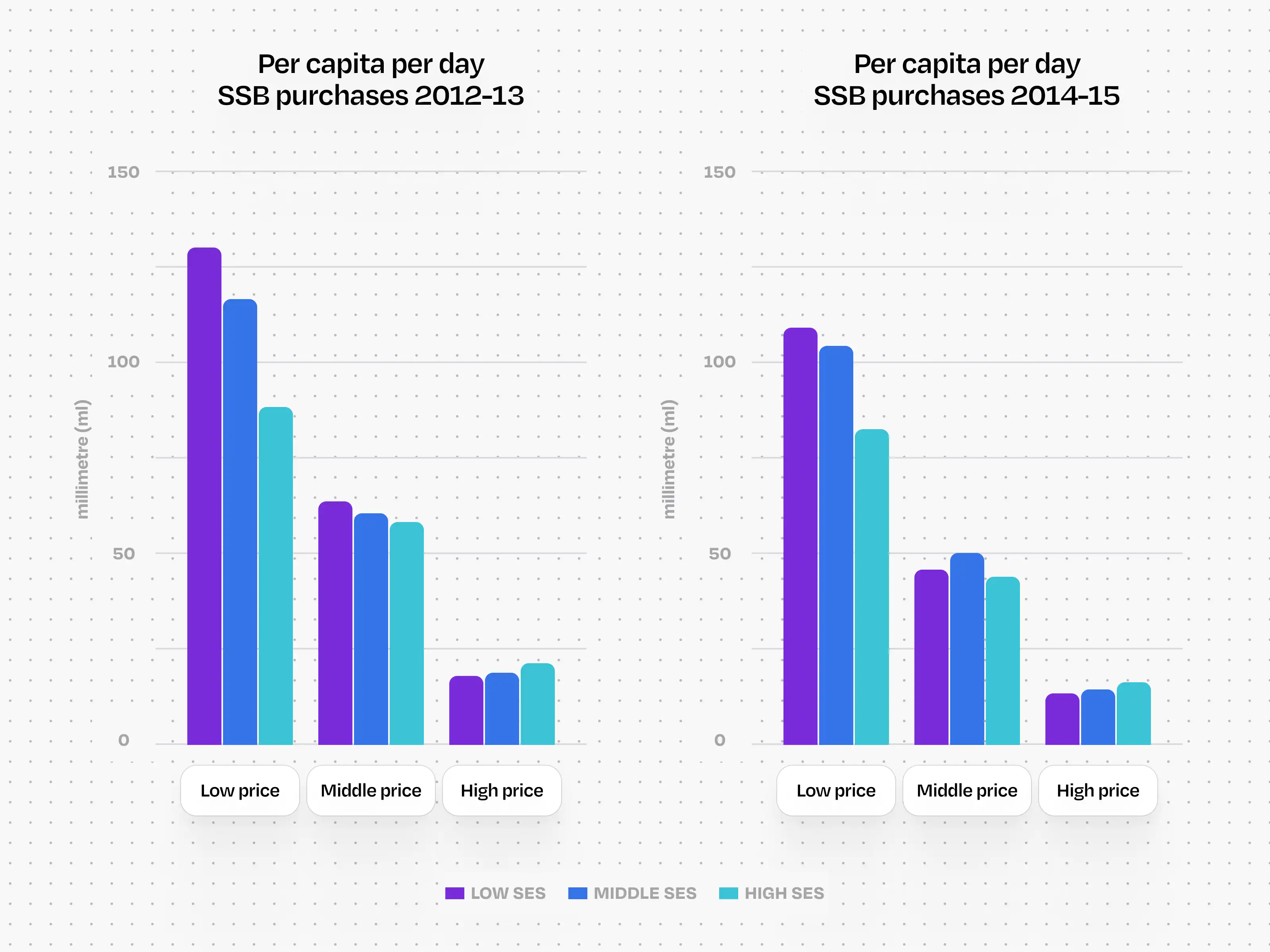
Despite early controversy, the campaign helped lower national soda purchases in the years that followed and remains one of the most studied obesity interventions in the Americas.
Chile’s Front of Pack Warning Labels
Chile pioneered one of the most influential policies in global nutrition reform. Packaged foods high in sugar, salt, or saturated fat must display black stop sign style warning labels. These labels were paired with restrictions on marketing to children and bans on selling such foods in schools.
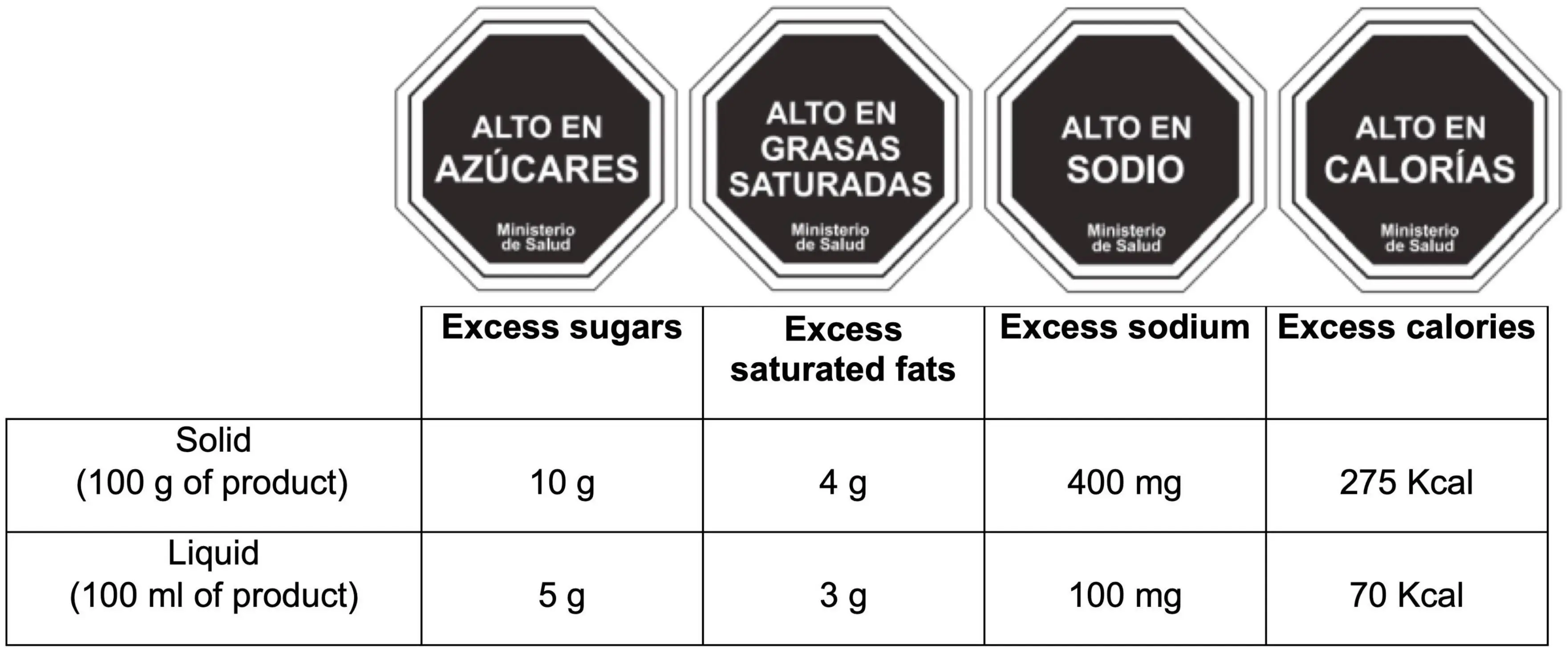
The model has spread across Latin America and parts of the Middle East. Studies show better consumer understanding of nutritional risk and measurable reductions in purchases of high sugar products.

Front-of-pack labels are simplified, high-visibility warnings placed directly on packaged foods to help consumers make quick, informed decisions at the point of purchase.
UK’s Change4Life
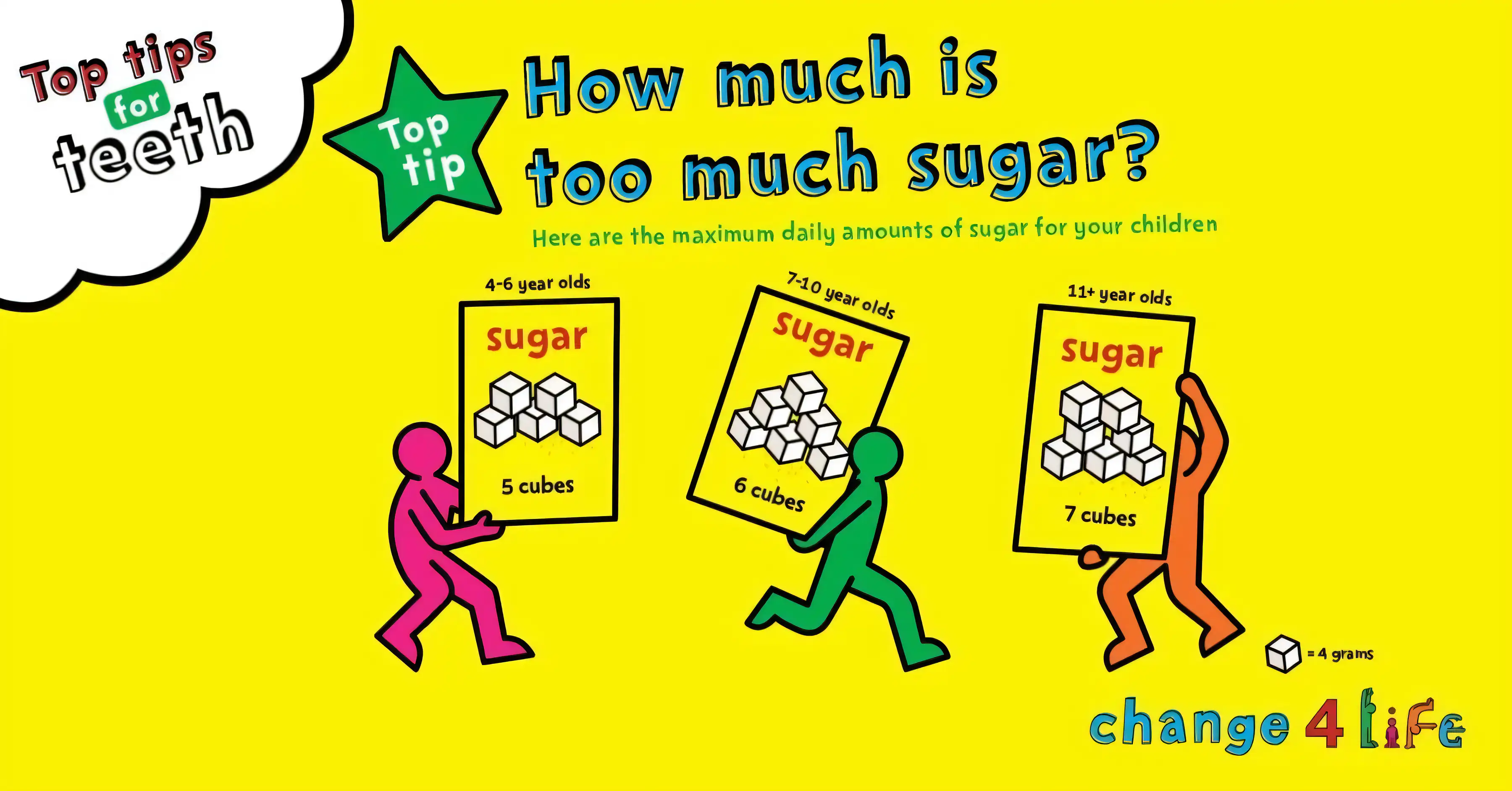
Launched in 2009, Change4Life was the UK’s first national social marketing campaign aimed purely at prevention. It focused on practical behaviors rather than weight loss. Importantly, the campaign deliberately avoided using the word “obesity,” based on research that positive framing is more effective than fear based messaging.
The campaign reached more than 99 percent of target families in its first year. Hundreds of thousands joined. Millions engaged with resources across television, print, digital, and community programs.
Key behaviors included eating five portions of fruits and vegetables daily, following the 400-600-600 calorie guideline for meals, reducing salt, and cutting high fat choices. Later, the “100 calorie snacks, two a day max” initiative targeted sugar reduction among children.
Results have been mixed, but Change4Life remains one of the most comprehensive government-led efforts in the world.
What are International Health Organizations to Create Awareness About Obesity?
World Health Organization Initiatives
At the 75th World Health Assembly in 2022, WHO members adopted major recommendations for obesity prevention and endorsed the WHO Acceleration Plan to Stop Obesity. The plan outlines priority actions, provides technical support to countries, and aims to reverse rising obesity rates by creating healthier systems.
The scale of the problem is severe. In 2021, obesity contributed to approximately 2.8 million noncommunicable disease deaths including cardiovascular conditions, diabetes, cancer, neurological disorders, respiratory disease, and digestive disorders.
In September 2025, the WHO and the UN Inter Agency Task Force recognized 12 countries and 7 non-state actors for pioneering multisectoral obesity action, from sugar taxes to national school meal programs.
World Obesity Day
Held every year on March 4, World Obesity Day encourages governments, clinicians, advocates, and the public to shift focus from individuals toward the systems that shape obesity risk. Health systems. Food systems. Media. Workplaces. Neighborhoods.
The 2024 campaign centered on youth-led conversations.
Countries also build their own national efforts, such as: • Singapore’s “One Healthy You,” focused on lifestyle risks • UAE’s “Stop the Weight of Stigma,” focused on discrimination
The Shift to ABCD: Redefining Obesity as a Medical Condition
One of the most important steps in reframing obesity is the adoption of Adiposity Based Chronic Disease, or ABCD, as the diagnostic term.
The traditional word “obesity” carries centuries of stigma. Its Latin origin meaning “to overeat” reinforces the misconception that obesity is about lack of willpower. ABCD reframes the condition in scientific terms. It positions obesity as a chronic metabolic disease rather than a problem of weight or discipline. Clinically, ABCD shifts treatment decisions away from weight alone and toward metabolic complications, risk profiles, and adipose function. It reflects total adiposity, fat distribution, fat function, and the complications that arise from dysfunctional fat over time.
ABCD also shifts the diagnosis away from BMI alone. It focuses on clinical severity, metabolic complications, and the physiological behavior of adipose tissue.
This approach reduces weight-centric bias and internalized stigma, both of which worsen health outcomes. Global medical bodies have begun endorsing ABCD, including the European Association for the Study of Obesity in 2019.

ABCD reframes obesity as a chronic metabolic condition rather than a weight problem.
The Economic Imperative
If nothing changes, global costs of overweight and obesity are projected to hit 3 trillion dollars per year by 2030 and more than 18 trillion dollars by 2060. These numbers explain why governments, pharmaceutical companies, and global institutions are investing heavily in prevention and treatment.
Challenges and Criticisms
Pharmaceutical campaigns face credibility challenges because companies profit from treatment. Messaging needs to walk the line between education and marketing. Novo Nordisk’s Spanish controversy shows how easily campaigns can backfire if they amplify fear instead of empathy.
Government campaigns struggle with socioeconomic disparities in behavior change. Some research on Change4Life shows limited long-term impact among higher-income groups. The decision to avoid the word “obesity,” while strategic, has been criticized as contradictory to the program’s goals.
International efforts face resource and infrastructure gaps, especially in low-income regions.

Global Signals
1 in 8 people now live with obesity worldwide. $3 trillion in projected global economic cost by 2030. Chile’s warning label law rewired an entire continent’s food policy.
What This Means for the Next Decade: Five Global Trends That Will Shape Obesity Communication by 2035
The campaigns of today are prototypes. The strategies that dominate the next decade will be shaped by technological acceleration, regulatory evolution, and cultural reckoning with systemic health inequity. Here are the five trends that will define obesity communication through 2035.
1. Pharma Marketing Will Pivot After GLP-1 Saturation
By 2028, the GLP-1 market will mature. Wegovy, Ozempic, Mounjaro, and Zepbound will face biosimilar competition, patent expirations, and consumer fatigue with injection-based therapies. The next wave of pharmaceutical marketing will focus on:
- Oral and long-acting formulations that reduce treatment burden
- Combination therapies targeting multiple metabolic pathways simultaneously
- Pediatric indications as early intervention become clinical standard
- Post-medication maintenance programs addressing weight regain after discontinuation
Expect campaigns to shift from "obesity is a disease" education (now widely accepted) to "sustained metabolic health requires integrated care" positioning. Companies will move further upstream into prevention, partnering with employers, insurers, and digital health platforms to own the full patient journey and not just the prescription moment.
The real battle will be narrative ownership. Whichever company successfully defines what "comprehensive metabolic care" means will capture the post-GLP-1 market. Lilly and Novo are already positioning for this with care ecosystem investments.
2. Governments Will Mandate Anti-Stigma Language in Public Health Communications
Following the ABCD adoption trajectory, expect regulatory bodies to formalize communication standards for obesity-related public health materials by 2030. This will include:
- Required use of person-first language ("person with obesity" vs "obese person") in government-funded campaigns
- Prohibited imagery guidelines similar to tobacco advertising restrictions, banning headless bodies and shame-based visuals
- Mandatory stakeholder review requiring patient advocacy groups to approve messaging before launch
Countries with national health systems (UK, Canada, Australia) will lead this shift. The U.S. will lag but see state-level adoption in progressive markets (California, New York, Massachusetts). Health departments that ignore these standards will face advocacy group litigation and public backlash.
This creates an opportunity for consulting firms and agencies that specialize in SEED Framework implementation. Governments will need external expertise to audit existing campaigns, retrain public health communicators, and redesign materials at scale.
3. AI-Powered Personalization Will Replace One-Size-Fits-All Campaigns
Mass media obesity campaigns will give way to hyper-personalized digital interventions powered by AI. By 2032, the dominant model will be:
- Behavioral phenotyping that segments audiences by metabolic profile, cultural context, health literacy, stigma exposure history, and readiness to change
- Dynamic content generation that adapts messaging tone, visual style, and information density in real-time based on user engagement signals
- Predictive intervention timing that delivers campaign touchpoints when individuals are most receptive (life transitions, health events, seasonal patterns)
Early movers like Noom and Omada Health are already testing these capabilities. The winners will be platforms that combine clinical precision with empathetic storytelling.
Technology that feels human, not algorithmic, will win.
Health communication is emotional, not mechanical; AI must respect this.
The challenge is algorithmic bias.
If training data reflects historical weight stigma, AI systems will perpetuate it. Ethical AI governance will become a competitive differentiator in health-tech obesity solutions.
4. Youth-Led Movements Will Redefine Body Autonomy and Medical Paternalism
GenZ and Gen Alpha are growing up in a world where body positivity, fat acceptance, and medical skepticism coexist with unprecedented obesity rates. By 2030, youth-led advocacy will force a reckoning:
- Rejection of top-down "obesity crisis" framing in favor of "health equity and systemic change" language
- Demand for patient autonomy in treatment decisions, pushing back against provider pressure to pursue weight loss
- Criticism of pharmaceutical marketing that medicalizes bodies without addressing root causes (food insecurity, environmental toxins, mental health)
Campaigns that succeed with this audience will co-create messaging with young people, center justice and autonomy, and avoid savior narratives. The WHO's 2024 youth-led World Obesity Day model will become standard, not exceptional.
Organizations that ignore this shift will face brand boycotts and influencer-led callouts. Gen Z holds companies accountable for values alignment, not just product efficacy.
5. Climate and Obesity Will Merge Into a Single Public Health Narrative
The food systems driving obesity are the same systems accelerating climate breakdown: industrial agriculture, ultra-processed foods, global supply chains optimized for profit over nutrition. By 2033, expect integrated campaigns that position sustainable eating as both climate action and metabolic health strategy.
This convergence will reframe obesity from individual disease to planetary health crisis, unlocking new funding streams, policy coalitions, and cultural narratives. Obesity becomes part of the Green New Deal. Carbon taxes become sugar taxes. Regenerative agriculture becomes preventive medicine.
The organizations that bridge these movements early, connecting climate activists, public health advocates, and food justice organizers, will lead the conversation. Those who treat obesity as isolated from environmental collapse will seem outdated.

Ultra-processed foods are industrial formulations engineered for shelf life, convenience, and low cost, which sit at the center of both problems.
These five trends point to a future where obesity communication is personalized, youth-driven, justice-oriented, algorithmically optimized, and ecologically integrated. The campaigns we see today are the last generation of mass-market, medicalized, institution-led initiatives. What comes next will be decentralized, co-created, and impossible to predict from a 2025 vantage point.
The only certainty: organizations that adapt fastest will define the field. Those that cling to 2020s models will be replaced.
Looking Forward
Obesity is now one of the world’s most urgent public health challenges.
The most effective path forward will likely combine:
- pharmaceutical innovation
- public policy and environmental reform
- culturally sensitive education and stigma reduction
- global collaboration and shared standards
Kenneth Custer of Lilly calls obesity a defining challenge of our time. More than one billion people are affected. Progress will require sustained action and alignment across sectors.
But the emerging campaigns show a clear trend. The world is finally treating obesity as a system level crisis rather than a personal failure. Only a comprehensive, multi dimensional approach will slow and eventually reverse the trajectory for future generations.
The question is no longer whether change will happen. The question is who will lead it and whether the solutions will arrive in time.
From Foresight
This essay is part of Foresight, Sparklin’s long-form publication exploring how global systems, stories, and campaigns shape human behaviour. Sparklin partners with organisations to design narratives, campaigns, and digital experiences grounded in research, empathy, and cultural intelligence.

Culture
Why Doctors Are Renaming Obesity to ABCD And What It Means for Healthcare, Stigma and Design
Obesity is getting a new name. ABCD: Adiposity-Based Chronic Disease, to shift the focus from stigma to science. The reframing chooses to recognize obesity as a complex, long-term medical condition, for better or for worse.

NOVA Food Classification Explained: How Ultra-Processed Foods Impact Your Health
Food labels have trained us to shop like accountants: subtract this, add that, hit the daily target. Food has lost its smell, its texture, its joy.

Emotional Carbonation: Gen Z’s Addiction to Diet Coke
It’s 3:17 PM. You’re deep in a task, halfway to burnout, and not really hungry, but there it is. That cold, familiar silver can waiting in the fridge. You crack it open not because you need it, but because it feels good. Because it marks the break. Because it’s yours. Because it has 0 calories. Once upon a time, this role belonged to the cigarette. Now? It’s Diet Coke.

Cognitive Gravity: Why New Ideas Feel Wrong Before They Feel Right
We don’t resist change because it’s wrong—we resist it because it feels wrong. From how we build cities to how we design technology, the best ideas often start by looking broken, and this essay explores why we cling to outdated systems long after they’ve stopped making sense.